Will the COVID-19 lockdown delay diagnosis of breast cancers?
Will the COVID-19 lockdown delay diagnosis of breast cancers?
Missed breast cancer diagnoses may become a tragic side-effect of women embracing advice to ‘stay home’

“One in seven women in Australia will be diagnosed with breast cancer in her lifetime. Early detection saves lives – the earlier a cancer is discovered, the greater the chance of successful treatment, with less aggressive treatment needed.” Source: Cancer Australia 2019
The impact of COVID-19
When Australian women were urged by public health officials to stay home, many became reluctant to see their GPs for non-urgent reasons. In addition, the switch to telehealth consultations has reduced the opportunity for GPs to conduct incidental breast checks, often performed when women present for another reason, such as for a prescription or a pap smear. Even women with breast symptoms, such as a lump or pain, have been reluctant to attend GPs, hospitals or radiology centres for fear of being exposed to COVID-19.
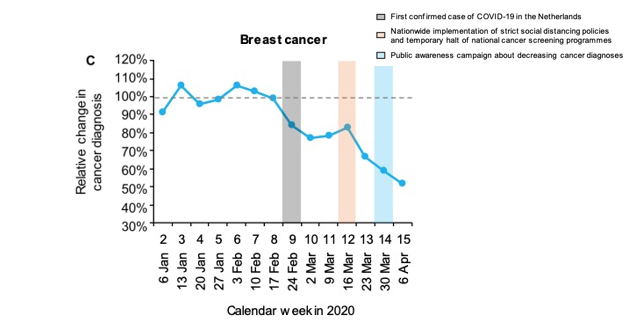
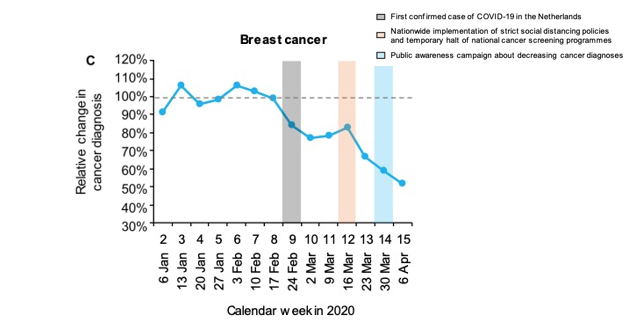
The Netherlands Cancer Registry reported a decline in cancer diagnosis of up to 40 per cent at the peak of the pandemic. In the figure below, the curve shows the country’s decline in breast cancer diagnoses since the start of 2020.1
Although there are no strictly comparable Australian data, there are health service data suggesting similar declines.
A delayed diagnosis may result in a breast cancer being diagnosed at a later stage – with an increased likelihood of more extensive surgery, radiotherapy and chemotherapy, as well as, possibly, a poorer outcome. It is particularly important that women with risk factors for breast cancer do not delay surveillance breast imaging because of COVID-19 fear.
Refer patients for a comprehensive risk assessment
General Practitioners should feel confident in assessing a woman’s breast cancer risk and referring her to an appropriate breast service for that woman’s needs. Diagnostic assessment, breast surveillance, and comprehensive risk assessment should not be postponed because of COVID-19 infection fear. In the current climate, in Australia at least, the effect of a delayed diagnosis is arguably a greater risk.
Keep in mind that the major risk factors for breast cancer2 are:
- having two or more first or second degree relatives diagnosed with breast or ovarian cancer (especially at a younger age),
- inheriting a known gene mutation that increases the risk of breast cancer (BRCA1, BRCA2, Li-Fraumeni or Cowden syndromes),
- not personally had testing, but having a first-degree relative with such a mutation,
- have been previously diagnosed with breast cancer or DCIS,
- having a lifetime risk of breast cancer of greater than 20% to 25%, according to risk assessment tools (based mainly on family history).
A less common, but significant risk factor is having had radiation therapy to the chest between the ages of 10 and 30 years, eg lymphoma treatment.
Modifiable risk factors include:
- nulliparity or first pregnancy after age 30,
- unable to or choosing not to breastfeed,
- MHT after menopause (especially when taken for 5 years or longer),
- weight gain after menopause,
- more than 2 standard alcoholic drinks a day,
- smoking in younger premenopausal women,
- eating a diet high in processed foods
For women at average risk of breast cancer, individualised surveillance is recommended.
For women at average risk, the need for additional tests, such as ultrasound, and the spacing of mammograms is determined by the mammographic density at each mammogram, and the results of any previous breast investigations.
It is difficult to generalise, but a common recommendation3 would be women between ages:
40 and 44: Baseline mammogram at age 40 with a discussion around starting regular mammographic surveillance.
45 and 54: mammogram every year.
55 and older: may be recommended to reduce to a mammogram every 18 months, every other year, or they may choose to continue yearly mammograms.
Screening should continue as long as a woman is in good health and is expected to live at least 10 more years.
Women who are at high risk for breast cancer based on the previously outlined factors, should begin annual screening with mammography +/- MRI around the age of 30 (or 10 years younger than their youngest affected relative) and continue for as long as they are in good health.
A woman at high breast cancer risk should make the decision to start breast surveillance with the aid of specific advice, taking into account her personal circumstances and preferences.
If MRI is used, it should be in addition to, not instead of, a mammogram. This is because MRI may still miss some cancers that a mammogram would detect, particularly DCIS.
About Sydney Breast Clinic
Sydney Breast Clinic is the only breast centre in Sydney offering same-day comprehensive assessment by breast specialists. Clinical examination and discussion with breast physicians and surgeons, mammograms read by specialised breast radiologists, ultrasound by breast sonographers, and, if necessary, needle biopsy, with examination of samples by breast cyto-pathologists. In a few hours, Sydney Breast Clinic can complete the gold standard ‘Triple Test’ (clinical examination, imaging and biopsy). These tests might take days or weeks in other settings.
Experienced Breast Physicians give a preliminary biopsy result to women within minutes of the biopsy being performed. The findings of all examinations are correlated and discussed with the patient and her GP on the day of her visit. If cancer is diagnosed, supportive counselling is provided. Resources are available to help women understand their diagnosis and obtain optimal treatment.
Sydney Breast Clinic has responded efficiently to the COVID-19 pandemic. Strict health and safety precautions are followed, maintaining high hygiene standards, including practising proper hand and equipment sanitising procedures between patients, and using gloves and masks where appropriate.
Sydney Breast Clinic is located in the CBD – easily accessed by car, train or bus. It is a stand-alone clinic, meaning that women can access breast examination and imaging without exposure to the COVID-19 risks of a hospital setting.
Who should you refer to Sydney Breast Clinic?
While Sydney Breast Clinic welcomes all referrals, this multi-specialist practice is particularly suited to women whose needs might not be fully met by other breast imaging services.
These women might have:
- a new breast symptom;
- a strong family history or other breast cancer risk factors;
- dense breasts – an independent risk factor for breast cancer;
- be seeking a second opinion or an in-depth risk assessment;
- breast implants;
- require monitoring of benign breast disease;
- had previous breast cancer or a previous breast biopsy suggesting an increased risk of breast cancer;
- breastfeeding issues, such as recurrent mastitis or an abscess requiring urgent drainage;
- painful cysts, requiring urgent drainage; or
- an increased likelihood of breast cancer for other reasons, such as HRT, chest irradiation, or DES exposure in utero.
Sydney Breast Clinic has responded to the COVID-19 pandemic by temporarily significantly reducing the out of pocket fee. Please, either note on the referral or phone if you have a patient who you believe is at risk and would need the fee (currently $295) further reduced.
Missed breast cancer diagnoses may become a tragic side-effect of women embracing advice to ‘stay home’
“One in seven women in Australia will be diagnosed with breast cancer in her lifetime. Early detection saves lives – the earlier a cancer is discovered, the greater the chance of successful treatment, with less aggressive treatment needed.” Source: Cancer Australia 2019

The impact of COVID-19
When Australian women were urged by public health officials to stay home, many became reluctant to see their GPs for non-urgent reasons. In addition, the switch to telehealth consultations has reduced the opportunity for GPs to conduct incidental breast checks, often performed when women present for another reason, such as for a prescription or a pap smear. Even women with breast symptoms, such as a lump or pain, have been reluctant to attend GPs, hospitals or radiology centres for fear of being exposed to COVID-19.
The Netherlands Cancer Registry reported a decline in cancer diagnosis of up to 40 per cent at the peak of the pandemic. In the figure below, the curve shows the country’s decline in breast cancer diagnoses since the start of 2020.1
Although there are no strictly comparable Australian data, there are health service data suggesting similar declines.
A delayed diagnosis may result in a breast cancer being diagnosed at a later stage – with an increased likelihood of more extensive surgery, radiotherapy and chemotherapy, as well as, possibly, a poorer outcome. It is particularly important that women with risk factors for breast cancer do not delay surveillance breast imaging because of COVID-19 fear.
Refer patients for a comprehensive risk assessment
General Practitioners should feel confident in assessing a woman’s breast cancer risk and referring her to an appropriate breast service for that woman’s needs. Diagnostic assessment, breast surveillance, and comprehensive risk assessment should not be postponed because of COVID-19 infection fear. In the current climate, in Australia at least, the effect of a delayed diagnosis is arguably a greater risk.
Keep in mind that the major risk factors for breast cancer2 are:
- having two or more first or second degree relatives diagnosed with breast or ovarian cancer (especially at a younger age),
- inheriting a known gene mutation that increases the risk of breast cancer (BRCA1, BRCA2, Li-Fraumeni or Cowden syndromes),
- not personally had testing, but having a first-degree relative with such a mutation,
- have been previously diagnosed with breast cancer or DCIS,
- having a lifetime risk of breast cancer of greater than 20% to 25%, according to risk assessment tools (based mainly on family history).
A less common, but significant risk factor is having had radiation therapy to the chest between the ages of 10 and 30 years, eg lymphoma treatment.
Modifiable risk factors include:
- nulliparity or first pregnancy after age 30,
- unable to or choosing not to breastfeed,
- MHT after menopause (especially when taken for 5 years or longer),
- weight gain after menopause,
- more than 2 standard alcoholic drinks a day,
- smoking in younger premenopausal women,
- eating a diet high in processed foods
For women at average risk of breast cancer, individualised surveillance is recommended.
For women at average risk, the need for additional tests, such as ultrasound, and the spacing of mammograms is determined by the mammographic density at each mammogram, and the results of any previous breast investigations.
It is difficult to generalise, but a common recommendation3 would be women between ages:
40 and 44: Baseline mammogram at age 40 with a discussion around starting regular mammographic surveillance.
45 and 54: mammogram every year.
55 and older: may be recommended to reduce to a mammogram every 18 months, every other year, or they may choose to continue yearly mammograms.
Screening should continue as long as a woman is in good health and is expected to live at least 10 more years.
Women who are at high risk for breast cancer based on the previously outlined factors, should begin annual screening with mammography +/- MRI around the age of 30 (or 10 years younger than their youngest affected relative) and continue for as long as they are in good health.
A woman at high breast cancer risk should make the decision to start breast surveillance with the aid of specific advice, taking into account her personal circumstances and preferences.
If MRI is used, it should be in addition to, not instead of, a mammogram. This is because MRI may still miss some cancers that a mammogram would detect, particularly DCIS.
About Sydney Breast Clinic
Sydney Breast Clinic is the only breast centre in Sydney offering same-day comprehensive assessment by breast specialists. Clinical examination and discussion with breast physicians and surgeons, mammograms read by specialised breast radiologists, ultrasound by breast sonographers, and, if necessary, needle biopsy, with examination of samples by breast cyto-pathologists. In a few hours, Sydney Breast Clinic can complete the gold standard ‘Triple Test’ (clinical examination, imaging and biopsy). These tests might take days or weeks in other settings.
Experienced Breast Physicians give a preliminary biopsy result to women within minutes of the biopsy being performed. The findings of all examinations are correlated and discussed with the patient and her GP on the day of her visit. If cancer is diagnosed, supportive counselling is provided. Resources are available to help women understand their diagnosis and obtain optimal treatment.
Sydney Breast Clinic has responded efficiently to the COVID-19 pandemic. Strict health and safety precautions are followed, maintaining high hygiene standards, including practising proper hand and equipment sanitising procedures between patients, and using gloves and masks where appropriate.
Sydney Breast Clinic is located in the CBD – easily accessed by car, train or bus. It is a stand-alone clinic, meaning that women can access breast examination and imaging without exposure to the COVID-19 risks of a hospital setting.
Who should you refer to Sydney Breast Clinic?
While Sydney Breast Clinic welcomes all referrals, this multi-specialist practice is particularly suited to women whose needs might not be fully met by other breast imaging services.
These women might have:
- a new breast symptom;
- a strong family history or other breast cancer risk factors;
- dense breasts – an independent risk factor for breast cancer;
- be seeking a second opinion or an in-depth risk assessment;
- breast implants;
- require monitoring of benign breast disease;
- had previous breast cancer or a previous breast biopsy suggesting an increased risk of breast cancer;
- breastfeeding issues, such as recurrent mastitis or an abscess requiring urgent drainage;
- painful cysts, requiring urgent drainage; or
- an increased likelihood of breast cancer for other reasons, such as HRT, chest irradiation, or DES exposure in utero.
Sydney Breast Clinic has responded to the COVID-19 pandemic by temporarily significantly reducing the out of pocket fee. Please, either note on the referral or phone if you have a patient who you believe is at risk and would need the fee (currently $295) further reduced.
References:
- Supplement to: Dinmohamed AG, Visser O, Verhoeven RHA, et al. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol 2020; published online April 30. http://dx.doi.org/10.1016/S1470-2045(20)30265-5.
- https://breastcancerriskfactors.gov.au/
- cancer.org/cancer/breast-cancer/
- Breast Cancer Risk Factors: A review of the evidence
- Population Attributable Risk of Modifiable and Non-modifiable Breast Cancer Risk Factors in Postmenopausal Breast Cancer. American Journal of Epidemiology 2016; 184 (12):884-893
- Reducing Breast Cancer Risk. Sydney Cancer Genetics website
References:
- Supplement to: Dinmohamed AG, Visser O, Verhoeven RHA, et al. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol 2020; published online April 30. http://dx.doi.org/10.1016/S1470-2045(20)30265-5.
- https://breastcancerriskfactors.gov.au/
- cancer.org/cancer/breast-cancer/
- Breast Cancer Risk Factors: A review of the evidence
- Population Attributable Risk of Modifiable and Non-modifiable Breast Cancer Risk Factors in Postmenopausal Breast Cancer. American Journal of Epidemiology 2016; 184 (12):884-893
- Reducing Breast Cancer Risk. Sydney Cancer Genetics website